Darwin College, the fight against COVID-19 and future Coronavirus Epidemics
Joint Vice-Master Professor Jonathan Heeney and his colleagues are working flat out on two streams of research they are concurrently running to understand immune responses that can protect us from SARS-CoV-2, and to develop a vaccine to protect against future epidemics like COVID-19.
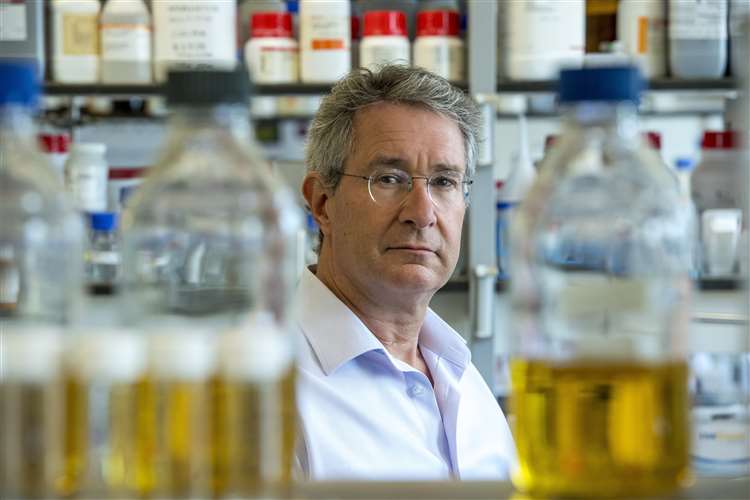
Clinical trials of a vaccine developed by Jonathan Heeney and colleagues in his lab could begin late in 2021 helped by an award of £1.9 million from the UK government. Professor Heeney who is head of the Laboratory of Viral Zoonotics at the University of Cambridge, and founder of DIOSynVax, a Cambridge University spinout company, says:
“Our approach involves 3D computer modelling of the SARS-CoV-2 virus’s structure. It uses information on the virus itself as well as its relatives – SARS, MERS and other coronaviruses carried by animals that threaten to ‘spill-over’ to humans again to cause future human epidemics.
We’re looking for chinks in its armour, crucial pieces of the virus that we can use to construct the vaccine to direct the immune response in the right direction, to the vulnerable weak spots of Coronaviruses. Ultimately, we aim to make a vaccine that will not only protect from SARS-CoV-2, but also other related coronaviruses.
Our strategy includes targeting those domains of the virus’s structure that are absolutely critical for docking with a cell, while avoiding the parts that could make things worse. What we end up with is a mimic, a synthetic part of the virus minus those non-essential elements that could trigger a bad immune response.”
While most vaccines use RNA or crippled viruses such as adenoviruses to deliver their antigens, DIOSynVax’s is based around a stable DNA copy that makes modified virus proteins that are seen as targets by the immune system. These synthetic gene inserts can also be placed within a number of different vaccine delivery systems that other companies are using including RNA. Once an antigen is identified, the key piece of genetic code that the virus uses to produce the essential parts of its structure is inserted into a DNA parcel known as a vector. The body’s immune cells take up the vector, decodes the DIOS-vaccine antigen and use the information to program the rest of the immune system to produce antibodies and T-cells against it. This DNA vector has already been shown to be safe and effective at stimulating an immune response against other pathogens and it is now being packaged into other vaccine delivery systems to demonstrate its versatility.
The vaccine in its DNA form can be freeze-dried as a powder which is heat stable, so does not need to be cold stored. Importantly, this makes the transport and storage of the vaccine straightforward – particularly important for distribution to low and middle-income countries where infrastructure is scarce, and populations are often remote.
The funding will allow the team to take the vaccine to clinical trial, which will take place at the National Institute for Health Research (NIHR) Southampton Clinical Research Facility at the University Hospital Southampton NHS Foundation Trust.
Concurrently, Professor Heeney is also instrumental in the national effort by UK immunologists to understand the protective immune responses to SARS-CoV-2, the coronavirus that causes COVID-19. In August this year the consortium, which is a collaboration led by Professor Heeney and Professor Wilhelm Schwaeble at the University of Cambridge, and Dr Helen Baxendale at the Royal Papworth Hospital NHS Trust, secured a grant of £1.5million for this important immune response research.
The funds allow the Humoral Immune Correlates of COVID-19 (HICC) Consortium to look at the role of antibodies in immunity to SARS-CoV-2 and characterise the antibody response in people who have mild or asymptomatic infection versus those who develop moderate or severe COVID-19 disease. The hope is to gain a better understanding of the differences between beneficial - or protective - antibody responses versus those that cause disease. This will help to determine why early indications suggest that people with stronger antibody responses may have had more life-threatening disease and what types of antibody responses are more effective in preventing severe infection.
Both studies together should push forward our understanding of the virus and how to combat it. The grants provided will make this process happen at an accelerated rate and human trials of the vaccine will start next year.

